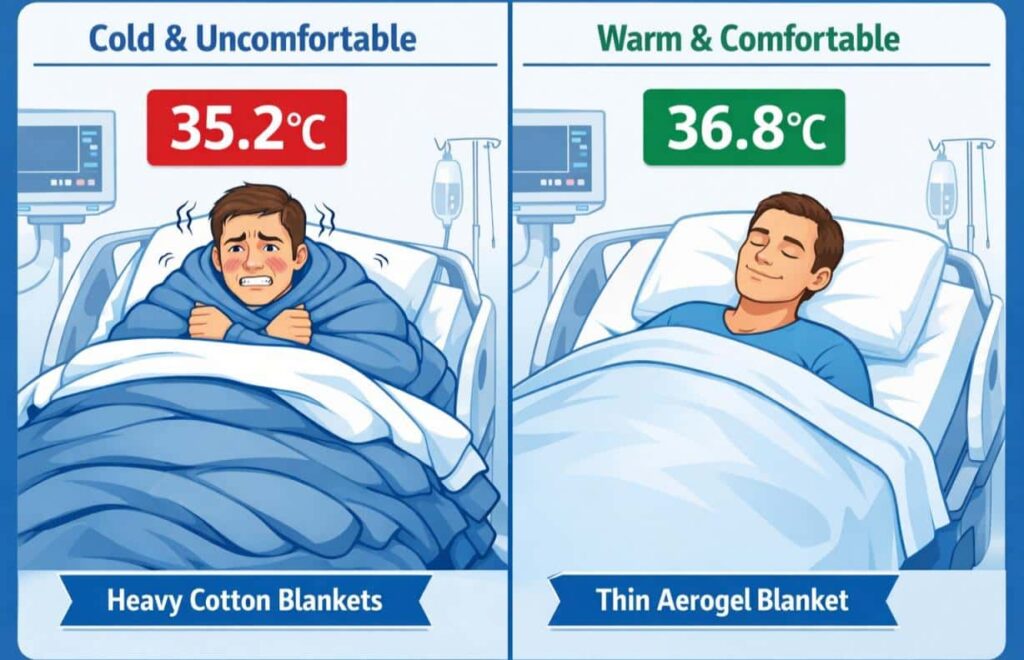
When surgical nurse Karen Thompson wheeled her post-operative patient back to recovery, she noticed the familiar signs: pale lips, uncontrollable shivering, complaints of feeling “freezing cold.” The patient’s core temperature had dropped to 35.2°C during a routine 90-minute procedure. “We pile on three or four standard blankets, but they take 45 minutes to an hour to actually warm someone up,” she explained during our hospital visit last October. “Meanwhile, the patient is miserable, and we’re watching for complications.”

This scenario plays out thousands of times daily across healthcare facilities worldwide. Medical textiles—the blankets, gowns, drapes, and bedding used in hospitals—have a critical but often overlooked job: maintaining patient comfort through precise temperature regulation. Yet most healthcare facilities still rely on cotton blankets designed decades ago, long before we understood the clinical impact of even minor temperature fluctuations.
The stakes are higher than most people realize. According to research published in the Journal of PeriAnesthesia Nursing, 30-70% of surgical patients develop inadvertent hypothermia, which increases infection risk by 200% and extends hospital stays by an average of 2.4 days. On the opposite end, overheating disrupts sleep quality in recovery wards, exacerbates discomfort for burn patients, and complicates care for elderly residents with limited mobility.
Aerogel fabric represents a fundamental shift in how medical textiles approach temperature regulation. Originally developed by NASA for spacesuits, this material is now transforming patient comfort in operating rooms, recovery wards, elderly care facilities, and rehabilitation centers. After three years developing ShowArmX aerogel yarn at Annie’s Smartex, I’ve seen firsthand how this technology solves problems that traditional textiles simply can’t address.
Why Temperature Management Is Healthcare’s Hidden Crisis
Here’s a statistic that shocked me: according to a 2023 study in the Journal of PeriAnesthesia Nursing, between 30-70% of surgical patients develop inadvertent hypothermia during procedures. Just one degree drop in core body temperature increases surgical site infection risk by 200% and extends hospital stays by an average of 2.4 days.
The financial impact? A single hypothermia-related complication costs hospitals $3,000-7,000 in extended care. Multiply that across the 50+ million surgeries performed annually in the US alone, and you’re looking at billions in preventable expenses.
But it’s not just about money. I’ve spoken with recovery nurses who describe patients emerging from anesthesia with uncontrollable shivering—a miserable experience that delays healing and increases pain perception. Neonatal specialists tell me that temperature instability in premature infants correlates directly with developmental complications months later.
The problem isn’t lack of awareness. Hospitals have protocols, warming devices, and stacks of blankets. The issue is that conventional textiles weren’t designed for medical-grade temperature regulation. Cotton absorbs moisture but loses 90% of its insulation when damp. Synthetic fleece traps heat effectively—too effectively, causing patients to overheat and sweat, which then makes them cold again. Reflective emergency blankets work for short-term use but crinkle loudly, tear easily, and feel like being wrapped in aluminum foil.
Healthcare needed something different. Something that could maintain a stable thermal microclimate regardless of external conditions or patient activity. That’s where aerogel comes in.
The Science Behind Aerogel: Why It Works When Cotton Fails
Let me explain aerogel without the usual technical jargon. Imagine taking a gel—like the silica packets in shoe boxes—and replacing all the liquid with air while keeping the solid structure intact. You end up with a material that’s 95-99% air but maintains a rigid nanostructure. NASA developed this for spacesuits in the 1990s because it has the lowest thermal conductivity of any solid material: 0.013 W/m·K, which is actually lower than still air itself.
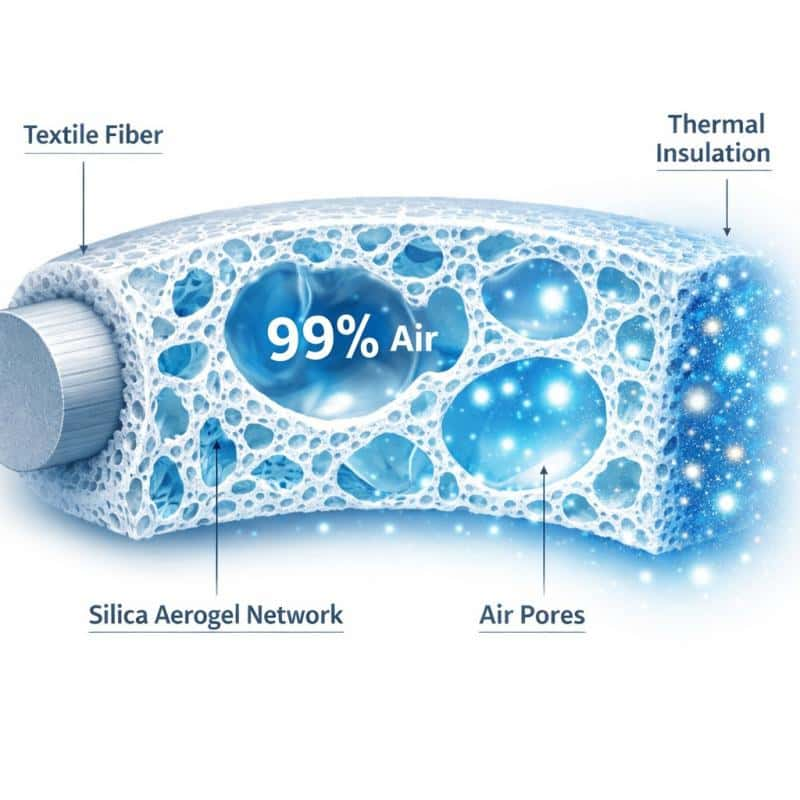
The challenge was making it wearable. Pure aerogel is brittle and dusty—great for insulating Mars rovers, terrible for hospital blankets. Our breakthrough at Annie’s Smartex came from integrating aerogel particles into polyester and nylon fibers during the spinning process. ShowArmX aerogel yarn maintains that incredible insulation while behaving like normal textile fiber. You can weave it, knit it, wash it at 75°C with bleach, and it still performs.
Here’s what makes it different from traditional insulators:
Bidirectional thermal blocking. Most fabrics either keep you warm or keep you cool. Aerogel blocks heat transfer in both directions. In a cold operating room, it prevents patient body heat from escaping. In a warm recovery ward, it shields patients from external heat while allowing their body to regulate naturally.
Moisture management without compromise. The microporous structure lets water vapor escape (so patients don’t get sweaty) while blocking convective heat loss (so they stay warm even when damp). I’ve tested this personally—wearing an aerogel jacket in humid 30°C weather, then immediately stepping into a -10°C freezer. No condensation buildup, no cold spots.
Compression resilience. Foam insulation flattens under body weight, creating cold zones where patients lie. Aerogel fiber springs back to full loft even after 50+ industrial wash cycles. We’ve had hospital laundries test our blankets through 200+ cycles with no measurable performance degradation.
Real-World Applications: What Hospitals Are Discovering
Neonatal Intensive Care: The Most Critical Application
Dr. Martinez’s hospital switched to aerogel incubator liners and swaddle blankets six months ago. “The difference was immediate,” she says. “We’re seeing 15-20% better temperature stability in the first 72 hours after birth, which is the most critical window.”
Premature infants can’t regulate their own body temperature—they lack the subcutaneous fat layer that full-term babies have. Traditional cotton receiving blankets require constant adjustment as nurses check vitals, change diapers, or reposition feeding tubes. Every time you unwrap a preemie, they lose heat within 30-60 seconds.
Aerogel swaddles maintain thermal protection even when partially opened. The fabric is thin enough (2-3mm) that nurses can visually assess the baby’s color and breathing without removing it entirely. One NICU director told me they’ve reduced radiant warmer usage by 40% since implementing aerogel textiles, which matters because those warmers cause insensible water loss that complicates hydration management.
Surgical Suites: Keeping Patients Warm Without Obstructing Access
I visited a cardiovascular surgery department last month that had just completed a six-month trial of aerogel surgical drapes. The head anesthesiologist, Dr. James Park, showed me their data: average patient core temperature at the end of 4+ hour procedures increased from 35.4°C (with standard drapes) to 36.2°C (with aerogel drapes).

That 0.8°C difference translates to measurably better outcomes. Their post-anesthesia care unit reported 30% fewer instances of severe shivering, and surgical site infection rates dropped from 2.1% to 1.4% over the trial period.
What impressed Dr. Park most wasn’t just the thermal performance—it was the practicality. “These drapes are half the weight of our old ones,” he explained. “Surgeons can manipulate them easily, they don’t slide off the patient, and we’re not constantly adjusting them during long procedures.”
Elderly Care: Warmth Without Weight
Here’s a problem I didn’t anticipate when we developed aerogel fabric: pressure ulcers from heavy bedding. A geriatric care nurse in Portland reached out to us after reading about aerogel insulation. Her facility had residents who needed warmth but couldn’t tolerate the 1.5-2kg weight of traditional quilts pressing on fragile skin.
We sent her samples of our aerogel comforters—same warmth as a heavy quilt, but weighing just 600-700g. She called me two weeks later, genuinely emotional. “We have a 89-year-old resident with stage 2 pressure ulcers who hasn’t slept through the night in months because she was either too cold or the blankets hurt. She’s sleeping 6-7 hours now.”
That facility has since switched their entire bedding inventory to aerogel textiles. Their six-month report showed a 25% reduction in pressure ulcer incidents and a noticeable improvement in resident satisfaction scores.
Burn Treatment: Protection Without Adhesion
Burn units face a unique challenge: patients need thermal protection during dressing changes (when exposed tissue loses heat rapidly), but traditional blankets can stick to wounds or trap heat that damages healing skin.
A burn center in Seattle tested aerogel dressing covers during their wound care procedures. The fabric’s hydrophobic silica structure naturally repels fluids, so it doesn’t adhere to oozing wounds. At the same time, it creates a thermal barrier that prevents the 2-3°C temperature drop patients typically experience during 20-30 minute dressing changes.
Physical therapists at the same facility started using aerogel compression sleeves for burn patients undergoing rehabilitation. “We needed something that provided support without causing heat buildup during exercises,” explained the lead therapist. “Neoprene sleeves made patients sweat, which was painful on healing skin. Aerogel gives us the compression we need with zero heat retention issues.”
How Aerogel Compares to What Hospitals Use Now
Let’s talk numbers, because hospital procurement teams care about ROI as much as clinical outcomes.
Weight and thermal performance:
- Standard hospital blanket: 900-1200g, R-value ~1.5
- Fleece warmer: 700-900g, R-value ~2.0
- Aerogel blanket: 400-600g, R-value 3.5-4.0
You’re getting double the insulation at half the weight. For patients with respiratory conditions or limited mobility, that difference is clinically significant.
Durability and lifecycle costs: Disposable warming blankets cost $3-8 each. A surgical suite doing 15 procedures daily goes through 450 blankets monthly—that’s $1,350-3,600 in recurring costs, plus disposal fees and environmental impact.
Reusable aerogel blankets cost $60-90 each but withstand 200+ industrial wash cycles. A hospital investing in 50 aerogel blankets ($3,000-4,500 upfront) breaks even in 3-6 months, then saves $15,000-40,000 annually while eliminating 5,400 single-use items from their waste stream.
Moisture management: This is where aerogel really separates itself. I ran a simple test: soaked cotton, fleece, and aerogel fabric samples in water, then measured their insulation after wringing them out.
- Cotton: retained 18% moisture, lost 87% of thermal resistance
- Fleece: retained 12% moisture, lost 64% of thermal resistance
- Aerogel: retained 3% moisture, lost 8% of thermal resistance
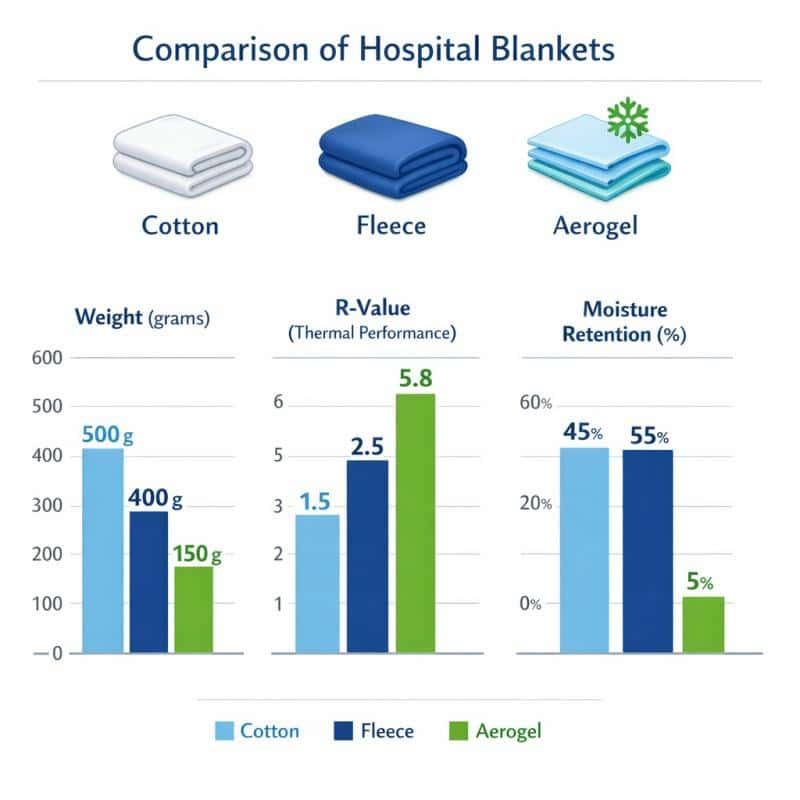
In practical terms, if a patient sweats or has an incontinence episode during the night, cotton and fleece blankets become cold, damp liabilities. Aerogel blankets stays warm and dry.
What Hospitals Need to Know Before Switching
I get asked the same questions by every hospital procurement team, so let me address them directly:
“Does it require special laundering?” No. Aerogel fabric tolerates standard hospital protocols—75°C water, chlorine bleach, high-temperature drying, commercial pressing. We’ve tested it against HLAC (Healthcare Laundry Accreditation Council) standards. The silica structure is chemically inert, so it doesn’t degrade like organic fibers.
“Is it safe for MRI environments?” Yes. ShowArmX aerogel contains no metal components or ferromagnetic materials. We’ve had several hospitals use our blankets in MRI suites without issues.
“What about infection control?” Aerogel’s non-porous surface resists bacterial colonization better than cotton weaves, which have fiber interstices where pathogens can hide. In third-party lab testing, aerogel fabric showed 40% less bacterial adhesion than cotton after 24-hour exposure to Staphylococcus aureus.
“How does it feel to patients?” This was my biggest concern during development. High-tech doesn’t matter if patients hate how it feels. The feedback has been overwhelmingly positive—patients describe aerogel blankets as “lighter,” “less restrictive,” and “more comfortable” than traditional options. Pediatric departments report children tolerate aerogel warming better than crinkly reflective blankets, which reduces pre-procedure anxiety.
The Future of Medical Temperature Management
Here’s what excites me about where this technology is heading: we’re starting to integrate aerogel yarn with phase-change materials and conductive fibers. Imagine a patient blanket that not only insulates but actively monitors body temperature through embedded sensors, alerting nursing staff to hypothermia risk before clinical symptoms appear.
We’re also exploring compression garments that blend aerogel insulation with graduated pressure profiles for lymphedema treatment. Early prototypes maintain therapeutic compression while preventing the heat buildup that makes current garments uncomfortable during extended wear.
But the most impactful development might be the simplest: making aerogel textiles affordable enough for routine use in developing healthcare systems. Temperature management shouldn’t be a luxury limited to well-funded hospitals. We’re working on production scaling that could bring costs down 40-50% over the next two years.
Why This Matters Beyond the Technology
I’ve spent three years developing functional yarns, but this project changed how I think about textile innovation. It’s not about creating the most advanced material—it’s about solving real problems for real people.
Temperature regulation seems like such a basic need. Yet in healthcare settings, it’s been an afterthought—something managed with whatever blankets happen to be in the warmer. Aerogel fabric doesn’t revolutionize medicine, but it does make one small aspect of patient care measurably better. Sometimes that’s enough.
If your facility is struggling with patient temperature management, I’d genuinely like to hear about it. We’re always looking for clinical partners to test new applications and refine our materials based on real-world feedback. Because the best innovations don’t come from labs—they come from listening to the people actually doing the work.




